While I’m a fan of Baby Led Weaning (BLW), the concern about not getting enough iron intake is real, especially since many moms like to offer fruits and veggies as starter foods for their babies. In fact, this is one of the top mistakes parents make when practising BLW!
Iron deficiency is estimated to be the most common deficiency worldwide. It can lead to anemia, impaired growth and development, as well as impaired cognitive function, including delayed attention, learning difficulties and social withdrawal. According to Malaysia’s National Health and Morbidity Survey (NHMS) 2022 Maternal and Child Health report, 46.5% of children between 0-5 years old were anemic. Therefore, in contrast to the popular saying, “food before 1 IS NOT just for fun.”
INCREASED NEEDS

By the age of 6 months, your baby’s iron stores, acquired during pregnancy, begin to deplete. This depletion is influenced by factors such as the mother’s iron levels during gestation, delayed cord clamping at birth, and the baby’s gestational age at birth. Around eighty percent of the baby’s iron stores accumulate during the third trimester of pregnancy. If your baby is born “overdue,” it can be one of the advantages in this context.
While breast milk contains a smaller quantity of iron (0.5 mg/L) compared to formula, but the iron present in breast milk is significantly more easily absorbed – approximately 50% absorption, as opposed to the 10% absorption rate in iron-fortified formula. Consequently, both breastfed and formula-fed infants receive comparable amounts of iron.
As infants reach six months of age, they continue to obtain some iron from their breast milk or formula, but introducing solid foods becomes crucial to provide a supplementary source. These solids are commonly referred to as “complementary foods,” as they complement the nutritional intake from a baby’s milk.
The question then arises: How much additional iron do babies require, and where should they get it from to ensure adequate intake?
HOW MUCH IRON DOES MY BABY NEED?

So, how much iron does a full-term, healthy-weight baby need?
In North America, the Recommended Dietary Allowances (RDA) for iron
- BABIES 0-6 MONTHS: 0.27 mg/day
- BABIES 6-12 MONTHS: 11 mg/day
- TODDLERS 1-3 YEARS: 7 mg/day
In Malaysia, The Recommended Nutrient Intake (RNI)
- BABIES 6-11 MONTHS: 9 mg/day (10% bioavailability); 6 mg/day (15% bioavailability)
- CHILDREN 1-6 YEARS: 6 mg/day (10% bioavailability); 4 mg/day (15% bioavailability)
Therefore, I think it depends where you are. The good aiming point is about 7-8 mg of iron daily for 6-12 month olds who consume meat. For vegetarian babies, a better target is probably 9-11 mg per day.
It is important to note that 11mg (RDA) is an average requirement (from breastmilk/formula and food) for ages 7 to 12 months. Babies’ iron needs don’t suddenly surge overnight, it’s a significant increase that we should strive to approach as quickly as possible. There can be a big difference in size and appetite between a 7 month old and a year old child. 12-month olds will need more iron than seven-month olds, but they can also eat more food, so they will work up to this amount gradually. The great news is that babies progress very quickly to consuming a fair amount of food with BLW.
Furthermore, you do not need to be counting the exact amount in milligrams of iron your child consumes each day – this is wearisome and stressful. The main goal is to provide as many iron-rich foods throughout the day as possible.
SIGNS OF IRON DEFICIENCY

If you’re worried that your child isn’t getting enough iron, here are some signs and symptoms of iron deficiency you can watch for:
- Slow weight gain
- Little or no appetite
- Pale skin
- Always tired
- Cold hands and feet
- Brittle nails
- Poor immunity (often sick or frequent infections)
To prevent anemia, the American Academy of Pediatrics recommends conducting a blood test on all 12-month-olds to assess their iron levels. In Malaysia, if you’ve concerns about your child’s iron intake or notice signs of deficiency, it is advisable to consult a doctor and request a blood test.
If the levels are significantly low, it is necessary to provide your child with iron supplements for a few months, as relying solely on food is unlikely to be enough to restore iron levels to normal levels.
CAN BABY LED WEANERS GET ENOUGH IRON (RESEARCH)

According to Baby-led Introduction to Starting SolidS (BLISS) study, two hundred families from New Zealand were divided into two groups: the BLISS group and the control group.
In the BLISS group, parents were taught to prevent choking, growth faltering and how tonsure an adequate intake of iron-rich foods while self-feeding. They were encouraged to offer at each meal:
- High iron food (e.g., red meat and fortified cereals)
- Energy-rich food (e.g., cheese or avocado)
- Easy-to-eat food ((e.g., fruit or veggie)
A study originating from the BLISS trial, titled “Impact of a Modified Version of Baby-Led Weaning on Iron Intake and Status: A Randomized Controlled Trial,” examined the effects. Nutrient intake at 7 and 12 months of age was assessed through weighted 3-day diet records. Additionally, the iron status of the babies was analyzed using a blood sample taken at 12 months of age.
The results indicated that 83% of babies in both the control and BLISS groups had adequate iron levels, with 5% in the control group and 7% in the BLISS group showing signs of anemia. No significant differences were observed between the two groups in terms of iron levels and stores at either 7 or 12 months of age.
This is indeed promising news! With additional education on the safe implementation of BLW, it has the potential to serve as a nutritious and safe approach to introducing solid foods.
So, Can BLW Babies Get Enough Iron?
The short answer is YES! It is possible.
The main source of iron for traditionally weaned babies is iron-fortified rice cereal, which is usually skipped in BLW. But, baby led weaners can absolutely get enough iron in their diets! In fact, BLW babies typically consume meat if it’s part of the family’s diet, whereas traditionally weaned babies might not eat meat right away at the beginning of starting solids. As long as parents focus on offering iron-rich foods at each meal, there is no significant difference in the iron status between babies following the BLW approach and those being fed purees.
Vegetarian and vegan infants might encounter more challenges in obtaining sufficient iron, yet this goal is achievable through strategic planning by parents. By conscientiously providing iron-rich foods or incorporating rice cereal, the necessary iron intake can still be achieved.
WHAT FOODS ARE HIGH IN IRON

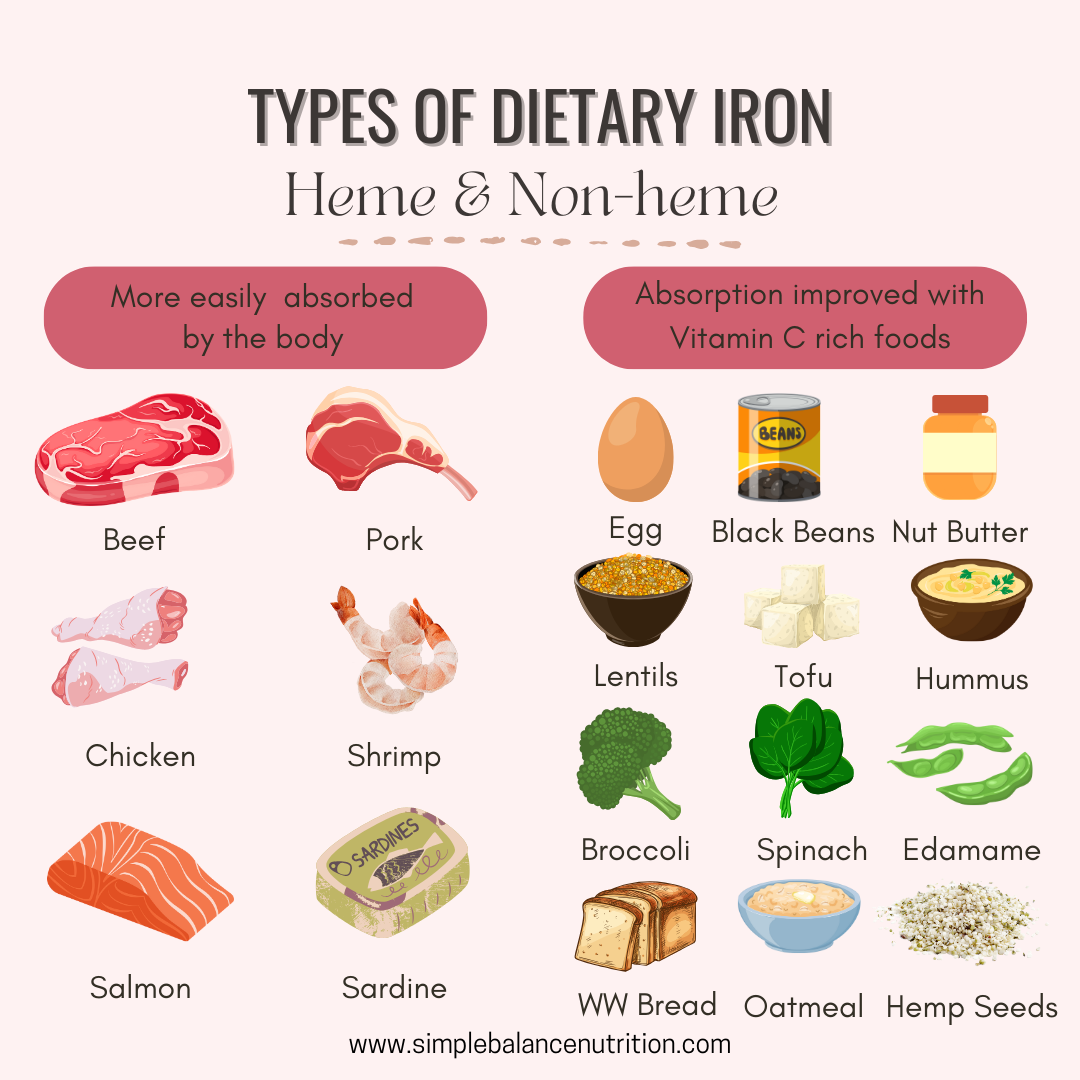
There are two types of iron sources: heme and non-heme. Heme iron, is found in animal products like meat, fish, and poultry, the human body has a high absorption rates at approximately 20%. Conversely, non-heme iron is found in plant sources like soy, lentils, beans, and even eggs, but it is less easily absorbed by the body, with only around 10% uptake. It is crucial to recognize that iron sources vary in their bioavailability.
I don’t believe in focussing on numbers and exact amounts of iron/foods to give, as this approach can lead to unnecessary stress. However, I do think it is useful to know the amounts of iron found in realistic serving sizes of some of the foods mentioned below. Here are a few examples along with approximate iron levels:
HEME-IRON FOODS:
- Liver (chicken, turkey, lamb), cooked* = 6.2-9.7 mg
- Ground beef (75 g) = 1.3-2.2 mg
- Ground chicken/pork (75 g) = 0.8-1.2 mg
- Chicken (75 g) = 0.4-2 mg (dark meat has higher levels than white meat)
- Sardines, canned (75 g) = 1.7-2.2 mg
- Tuna, light, canned in water (75 g) = 1.2 mg
*While liver is an excellent source of iron, it contains an excessive amount of preformed Vitamin A, which could be toxic. The Upper Limit recommended for ages up to 3 years is 600 micrograms, whereas just 1 oz of liver contains over 5,000 micrograms. Plus, the liver is the filter for our body, and it can also contain metals.
How to serve heme-iron foods in BLW:
- Ground meat sauce
- Baby burgers or meatballs
- Offer no-added salt canned sardines as finger food
- Pressure or slow-cooked pork or beef roast, shredded
- Pork ribs or chicken legs (removed of gristle)
- Boneless chicken thighs, cut into finger-sized strips
- Fish or salmon cakes
NON-HEME IRON FOODS:
- Eggs (2 eggs) – 1.2 – 1.8 mg
- Edamame (1/2 cup) = 1.9-2.4 mg
- Tofu (¾ cup) = 2.4-8 mg
- Lentils (¾ cup) = 4.1-4.9 mg
- Beans (white, kidney, navy, pinto, black, etc.) (¾ cup) = 2.6-4.9 mg
- Hummus (¼ cup) = 1.4 mg
- Oatmeal, instant, cooked (¾ cup) = 4.5-6.6 mg
- Wheat germ (1 tbsp) = 1.2 g
- Spinach, cooked (½ cup) = 2.0 -3.4 mg
- Hemp hearts (1 tbsp) = 1.4 mg
- Blackstrap molasses (1 tbsp) = 3.6 mg
How to serve non-heme iron foods in BLW:
- Eggs fried and sliced in strips or scrambled
- Firm tofu strips sautéed or roasted.
- Blend soft tofu into smoothies for variety.
- Add blackstrap molasses to baking.
- Sprinkle wheat germ or hemp hearts on yogurt or blend into a smoothie.
- Serve hummus on a strip of toast.
- Black beans are a good finger food to practice the pincer grasp.
- Smush larger beans like chickpeas with your finger, so they’re not a choking hazard.
- Bean or lentil patties.
- Nut butters on toast fingers.
TIPS TO GET ENOUGH IRON WHILE USING BLW (6-12 months)

- Continue providing adequate breast milk or formula as the baby’s main source of nutrients. At this age, solid foods serve as complimentary options to to boost baby’s nutrient intake and gradually prepare their digestive system for a complete transition to solids.
- Ensure that every meal includes a source of iron, both heme and non-heme iron.
- Incorporate fortified powder infant cereal baked into finger foods. You can also substitute half of the flour in your pancake recipes with fortified infant cereal.
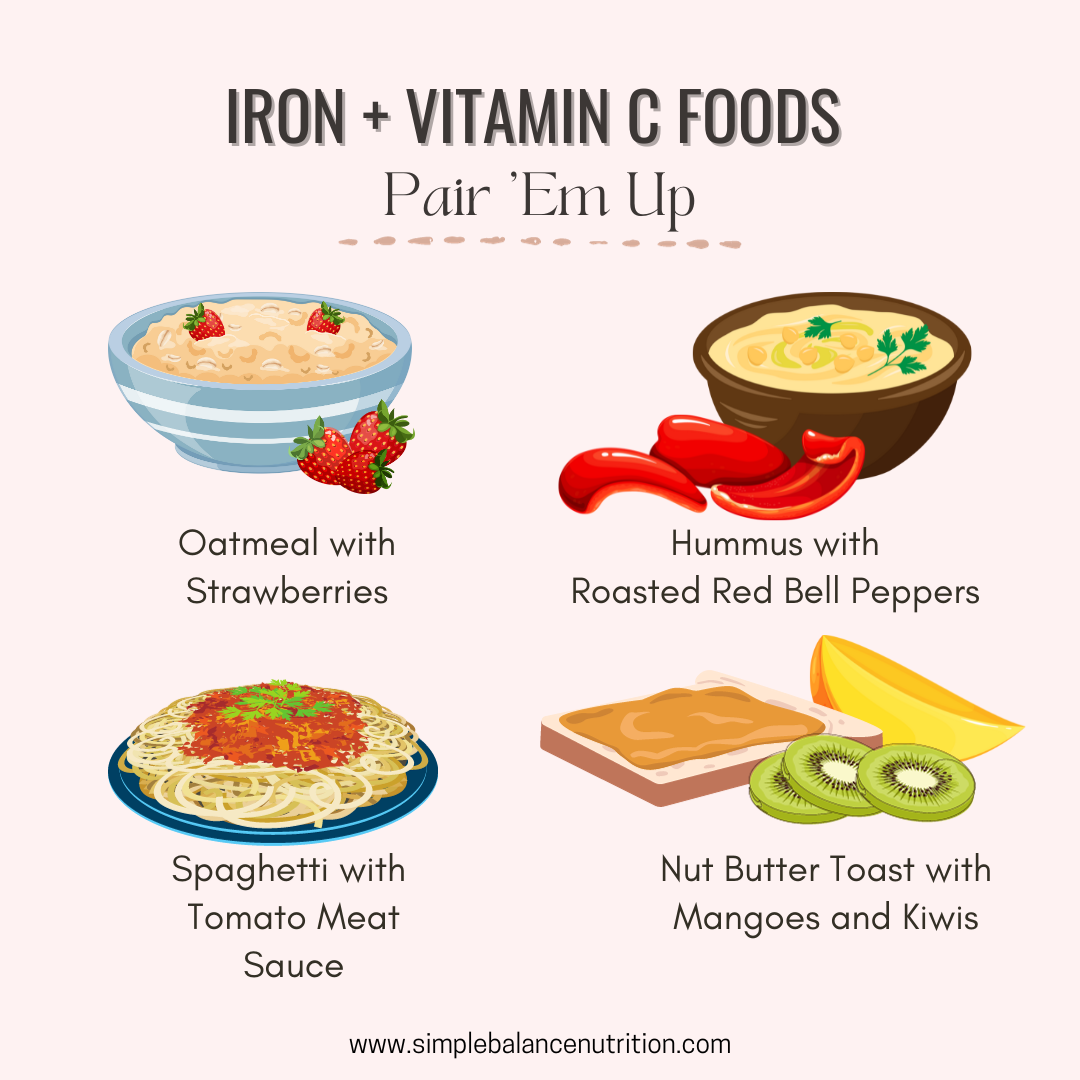
- Pair iron-rich foods with vitamin C rich foods, to increase the absorption of non-heme iron in the body. Consider top[ing fortified pancakes or cereal with fruit compote; serve lentils in stewed tomatoes and adding spinach to a fruit smoothie.
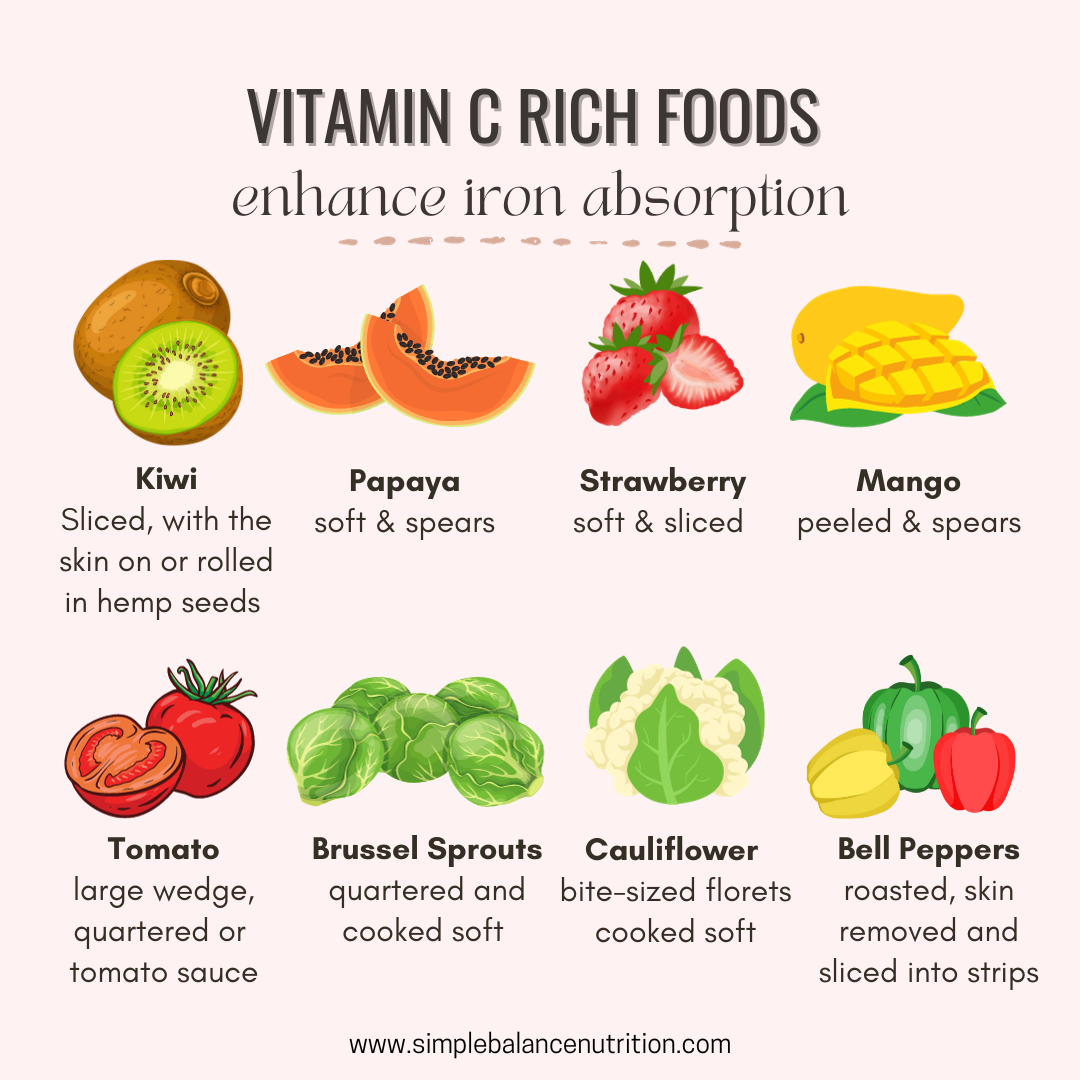 Other good sources of vitamin C, including bell peppers, tomatoes, broccoli, citrus fruit and berries, etc. Ground meat in a tomato-based sauce forms an ideal combination.
Other good sources of vitamin C, including bell peppers, tomatoes, broccoli, citrus fruit and berries, etc. Ground meat in a tomato-based sauce forms an ideal combination.
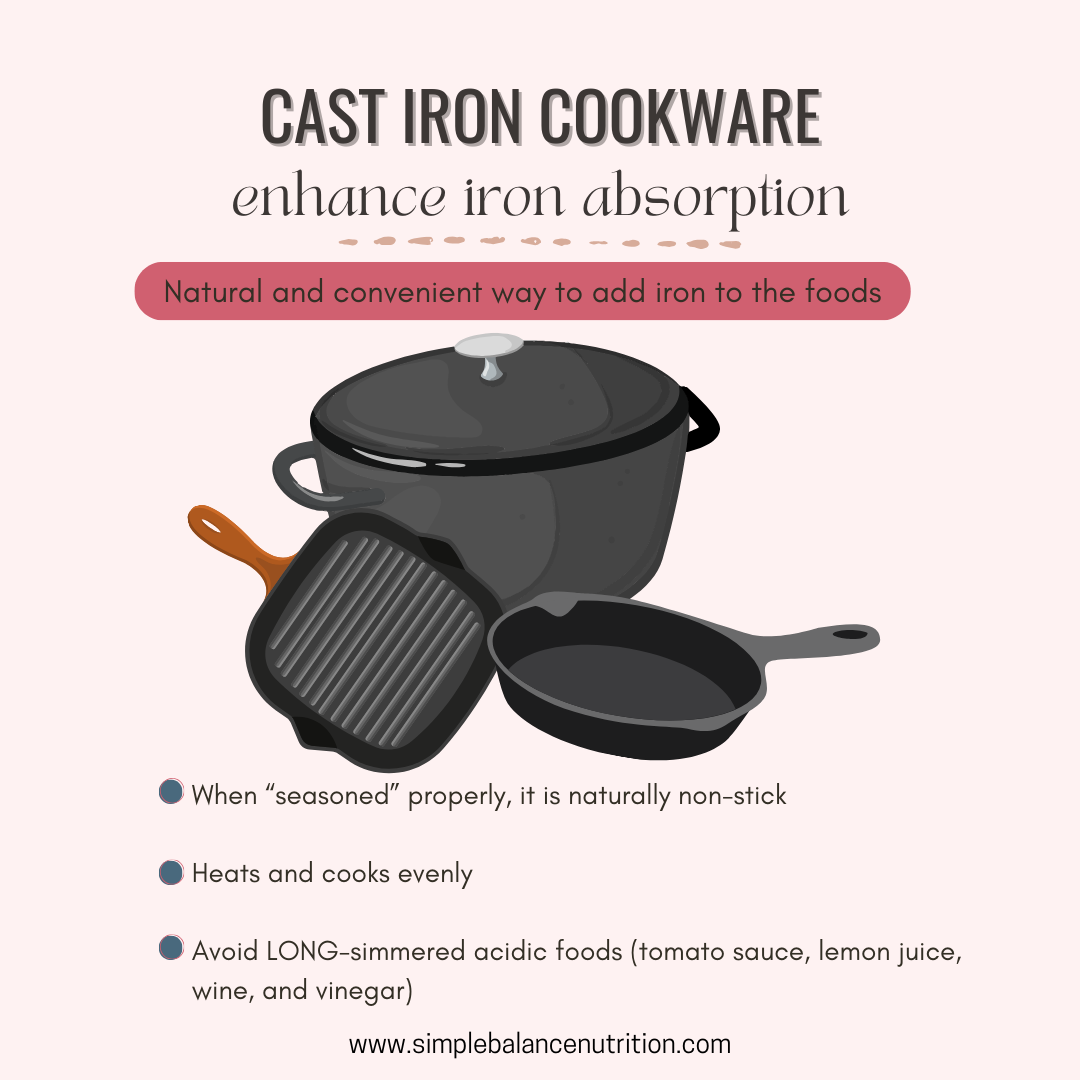
- Cook with cast iron cookware. Cooking with cast-iron pots and pans safely introduces additional iron to the prepared dishes. If you don’t have one, you can try a product called the Lucky Iron Fish®. This is a simple, reusable and effective cooking tool that adds extra iron to your daily foods, soups or drinks. It is an affordable solution, especially for those with iron deficiency anemia.
- Cook with garlic or onion. Preparing meals with allium-containing ingredients (such as garlic and onions) can help increase iron absorption.